by Dr. Shapira | Sep 3, 2017 | Blog
Patients with orofacial pain most commonly have myofascial pain but it is always important to remember that orofacial pain is the most frequent first symptom of Cardiac pain. This has been published in numerous locations including: Craniofacial Pain as Sole Prodromal...
by Dr. Shapira | Jul 1, 2014 | Blog
The wrong treatment for migraines can actually increase future risk for increased severity and frequency of migraine. Physiologic dentistry can decrease the severity and frequency of future migraines in many patients. The first step is a complete evaluation and the...
by Dr. Shapira | Apr 11, 2014 | Diagnosis of TMJ
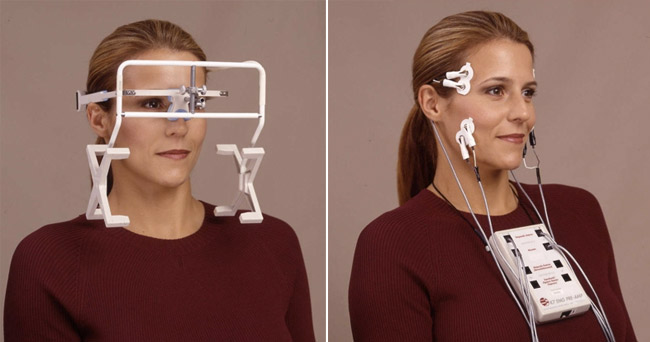
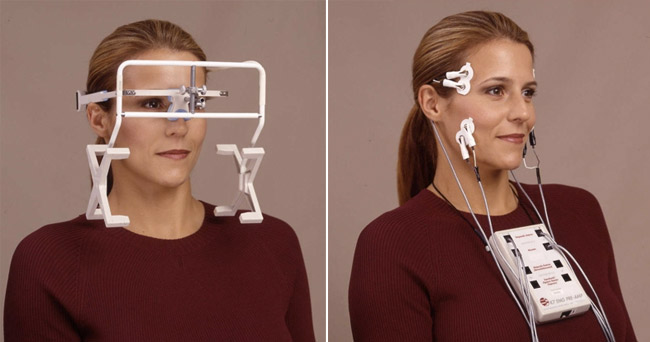
How TMJ Is Diagnosed By A Dentist Get to the root of your discomfort right here in the Chicago Area TMJ is a type of complex disorder that frequently goes undiagnosed or worse misdiagnosed. Patients feel that they can handle the popping they hear in their jaws when...